Therasoft Claims — Intelligent Billing for Modern Mental Health Agencies
Transform Your Mental Health Billing With AI-Powered Accuracy
Since 2008, Therasoft Claims has helped mental health agencies eliminate billing headaches and dramatically improve collections.
We combine advanced Artificial Intelligence, decades of industry expertise, and a full-time team of certified billers and coders to deliver a revenue cycle experience built for today’s outpatient world.(performance of our revenue management service speaks for itself)
Therasoft Claims ensures you get paid faster, more accurately, and with zero administrative stress.
Why Mental Health Agencies Choose
Therasoft Claims
Mental Health billing knowledge, experience and performance that sets us apart with a track record of 17 years
of helping therapists with our billing service.
AI-Powered Denial Management
Our proprietary AI engine analyzes claim data, payer patterns, and denial trends to predict, prevent, and resolve denials before they hurt your bottom line.
Automated denial detection
Smart re-submission workflows
Reduced AR days
Higher first-pass acceptance rates

One-Click Real-Time Eligibility
Instant eligibility and benefits verification for every major insurance plan
Verify coverage in seconds
Reduce no-pays
Improve scheduling confidence
Protect your clinical team from billing surprises

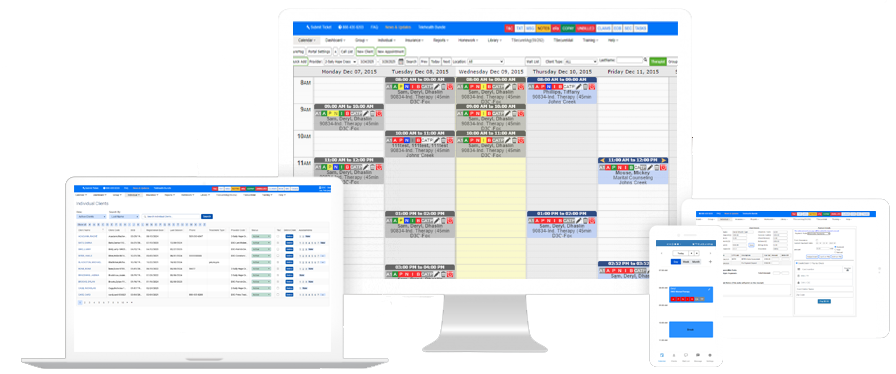
Rapid Claim Submission & Live Status Tracking
Our proprietary AI engine analyzes claim data, payer patterns, and denial trends to predict, prevent, and resolve denials before they hurt your bottom line.
Our RCM system lets you see exactly where your money is — from submission to payment posting.
Automated EOB Posting
AI-driven EOB reading and payment posting eliminates manual data entry errors.
Your financial reports are always clean, accurate, and up to date.

AI-Powered Error Scanning
Before any claim is submitted, our AI engine runs a deep compliance and coding audit. This ensures:
Zero missing data
Correct CPT/diagnosis codes
Maximum allowable reimbursement

Full-Time Billing & Coding Team
You don’t just get software — you get a complete billing department dedicated exclusively to mental health.
Our team handles everything:
Claims
Denials
Reconciliation
Secondary claims
Patient billing
Dedicated Account Manager
Every agency receives a single point of contact who knows your practice, your payers, and your financial goals.
No call centers. No tickets. Just real people delivering real results.

Trusted by Mental Health Agencies Since 2008
We process over one million claims every year across outpatient mental health, group practices, intensive outpatient programs, and multidisciplinary agencies.
Our long track record means you get the stability, accuracy, and professionalism your organization deserves.
Therasoft Claims is built for agencies that want:

The Future of Behavioral Health Billing Is Here
Artificial Intelligence. Human Expertise. Maximum Reimbursement.
Therasoft Claims is where cutting-edge automation meets real-world billing mastery.
If you're ready to eliminate denials, streamline your operations, and take control of your revenue cycle, we’re ready to help.